Insulin Pump Therapy
Insulin Pump Therapy delivers insulin continuously through a small wearable device, helping people with diabetes manage blood sugar more precisely and flexibly than multiple daily injections.
This content is not medical advice. Always consult your endocrinologist, doctor or diabetes care team before making any changes to your diabetes treatment or daily management.
What Is an Insulin Pump?
An insulin pump is a small, computerized device that delivers fast-acting insulin through a thin cannula inserted under the skin. The pump is usually worn on the body and provides continuous basal insulin as well as bolus doses when eating or correcting high blood sugar. Unlike multiple daily injections, the insulin pump automates much of the process and can be programmed to match an individual’s needs. Today, more than one million people worldwide use insulin pump therapy, with an estimated 350,000 to 515,000 users in the United States. (ADCES, 2025)
History of Insulin Pumps
1970’s – The beginning: the first pumps were bulky, backpack-sized devices used mainly in hospitals for research.
1980’s and 1990’s – Miniaturization: pumps became portable, safer, and more user-friendly, allowing patients to wear them daily.
2000’s – Advanced features: touchscreens, programmable basal rates, alarms, and waterproof options improved flexibility.
Today – Smart systems: modern pumps integrate with Continuous Glucose Monitoring (CGM) devices and use algorithms to automatically adjust insulin delivery.

Why Choose Insulin Pump Therapy?
The number of people using insulin pumps is steadily growing worldwide. Pump therapy offers benefits such as:
Greater flexibility in eating and daily routines
Reduced risk of hypoglycemia and extreme highs
Improved HbA1c and time-in-range outcomes in clinical studies
Better quality of life for children, teens, and adults with diabetes
Everyday Use and Safety Features
Modern insulin pumps go beyond simply replacing multiple daily injections. They allow very fine adjustments of insulin doses, even in increments as small as 0.1 units or less making therapy safer for children and people highly sensitive to insulin. Basal delivery can be temporarily increased or decreased, for example during illness or physical activity, and in some cases even suspended for short periods.
Some pumps also connect with Continuous Glucose Monitoring (CGM) systems for added safety. More details on CGM integration are provided in the section below.
Safety features are built into every device: alarms for occluded infusion sets, empty reservoirs, or low battery alerts. Insulin reservoirs are typically changed every 2–3 days, and infusion sets are replaced regularly to ensure both effectiveness and safety.
Battery and charging options vary by model. Some pumps use standard AA or AAA batteries that last 2–4 weeks, while newer pumps feature rechargeable batteries that are powered via USB and usually last several days up to a week. In both cases, pumps give clear warnings so users can replace or recharge in time.
By combining precision, flexibility, and safety, insulin pumps have become one of the most advanced therapy options for type 1 diabetes, enabling people to manage their condition with greater freedom and confidence.
Types of Insulin Pumps
People with diabetes today have access to a variety of insulin pumps, each designed to meet different needs and lifestyles. While all pumps share the goal of delivering insulin continuously, their features, designs, and technology can vary significantly. Below are the most common types of insulin pumps available:
1. Traditional Insulin Pump
A traditional insulin pump delivers a steady basal rate of insulin throughout the day and allows users to give bolus doses for meals or to correct high blood sugar. These pumps use rapid-acting insulin and connect to the body through a small cannula placed under the skin with an infusion set. They typically have larger insulin reservoirs and multiple programmable settings for flexibility.
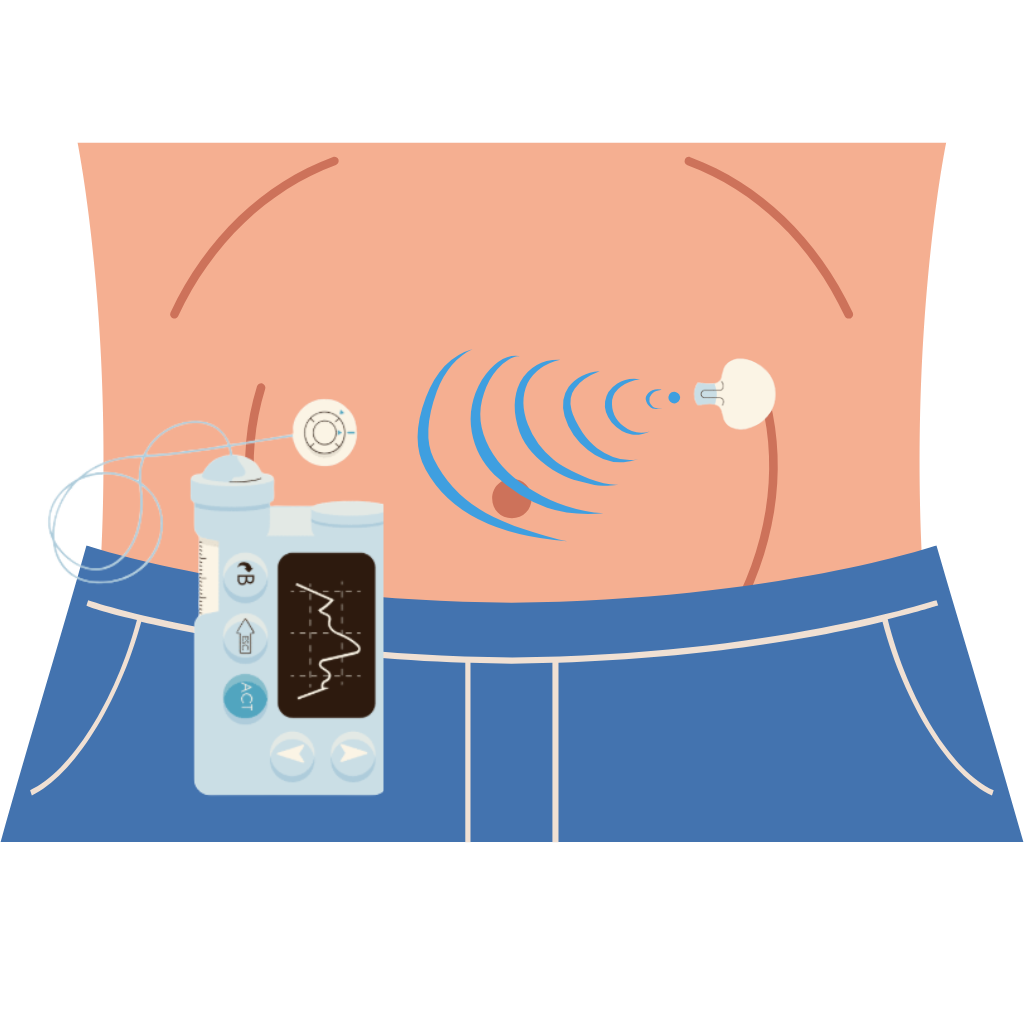
2. Patch (Tubeless) Pump
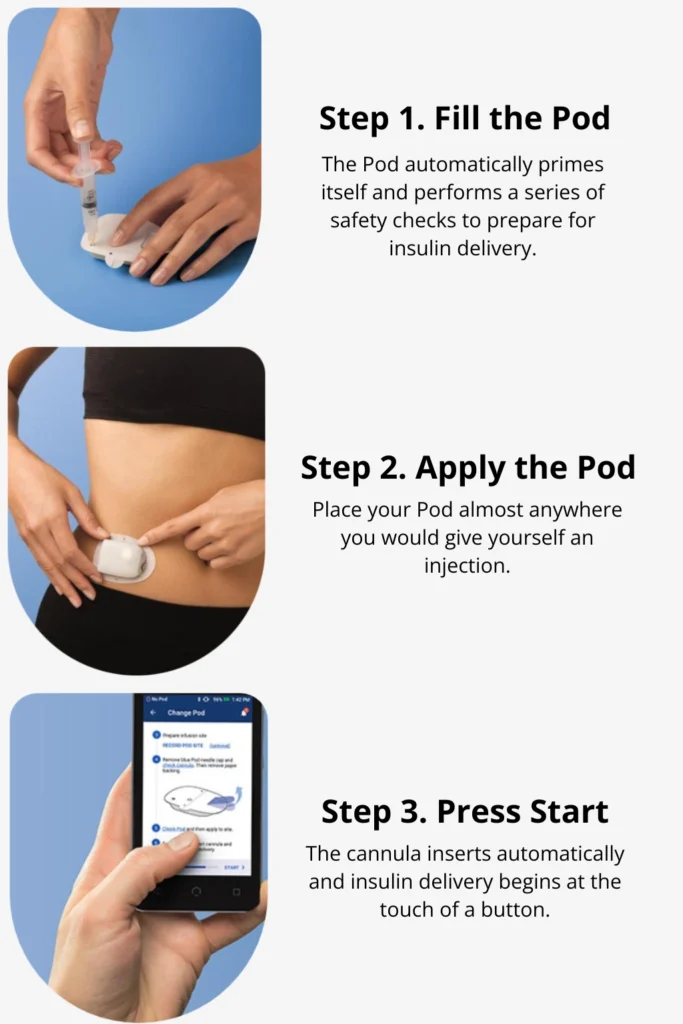
Patch pumps are tubeless devices that adhere directly to the skin and contain both the insulin reservoir and cannula in a single unit. They are usually controlled wirelessly through a separate controller or smartphone app. Their discreet design makes them popular among users who prefer not to manage tubing. A well-known example is the Omnipod.
Note: all patch pumps are tubeless, but not all tubeless pumps are patch-style. Some tubeless pumps are designed differently, though patch designs are the most widely available.
3. Hybrid Closed-Loop Systems
Often referred to as “artificial pancreas” systems, these pumps work in combination with continuous glucose monitoring (CGM) devices. Using real-time glucose data, they automatically adjust basal insulin delivery and, in some cases, correction doses. This technology significantly reduces the burden of diabetes management and helps maintain blood sugar within target ranges. Examples include the Medtronic 780G, Tandem Control-IQ, and Beta Bionics iLet.
4. Disposable Insulin Pump
Disposable pumps are short-term solutions, designed to be worn for a few days or weeks before being discarded. They are often more affordable and are a good option for people who want to try pump therapy without a long-term commitment.
5. Integrated Insulin Pump
Some pumps are fully integrated with CGM technology in a single device. Integration allows for automatic insulin adjustments based on glucose data, making therapy more seamless. This reduces the need for constant manual input and provides tighter glucose control.
6. Bluetooth-Enabled Insulin Pump
Many modern pumps come with Bluetooth connectivity, allowing users to pair the pump with smartphones or other devices. This feature enables remote monitoring, easier adjustments, and data sharing with healthcare providers. It also adds convenience for users who prefer managing therapy through their phone.
7. Mini-Dose Insulin Pump
Mini-dose pumps are designed for individuals who need very small, precise amounts of insulin — such as children or people with high insulin sensitivity. These pumps can deliver extremely fine increments, ensuring accurate dosing and better safety for sensitive patients.
When considering insulin pump therapy, it is important to explore all available options and features to find the device that best fits your lifestyle, medical needs, and local availability. Proper training is just as important as the pump itself. Learning how to adjust settings, respond to alarms, and manage infusion sites ensures safe and effective use. Education provided by diabetes care teams helps users gain confidence and achieve the best results from pump therapy.
Latest and Notable Insulin Pumps
Insulin pump technology is rapidly advancing, with new models offering smaller size, longer battery life, wireless charging, and greater integration with CGM systems. By 2025, several next-generation pumps are available, while others are in rollout phases across different markets.
Popular Insulin Pump Options
Medtronic MiniMed 780G – hybrid closed-loop pump with advanced algorithms, automatic corrections, and CGM integration.
Tandem t:slim X2 with Control-IQ – touchscreen pump with automated insulin delivery, remote software updates, and Dexcom CGM compatibility.
Omnipod 5 – tubeless, patch-style pump connected to Dexcom G6/G7, offering discreet use and automated dosing.
Roche Accu-Chek Solo – patch pump with modular design, detachable cannula, and remote control features.
Ypsomed YpsoDose – slim pump with easy-to-use menus, Bluetooth connectivity, and growing integration with CGMs.
SOOIL Dana-i / Dana RS – lightweight pumps designed for app-based control and open protocol use.
Medtrum A7+ TouchCare – patch pump with AID features and compatibility with Medtrum CGM systems.
Beta Bionics iLet Bionic Pancreas – dual-hormone pump (insulin + glucagon) designed to fully automate glucose regulation.
Important Notes on Availability
✅ Varies by region – some pumps are FDA-approved in the U.S., while others are available only in Europe or Asia.
✅ Insurance coverage – cost and access depend heavily on health insurance or out-of-pocket payment.
✅ CGM compatibility – pump performance often depends on which CGM devices it integrates with.
✅ Consult your care team – the best pump for you depends on diabetes type, therapy needs, lifestyle, and local availability.
Insulin pumps are most effective when used together with continuous glucose monitoring (CGM) systems. By sharing real-time glucose data, pumps can automatically adjust insulin delivery, creating a more seamless and personalized therapy. To explore how CGM works, its latest innovations, and why it matters alongside insulin pumps, visit our dedicated Continuous Glucose Monitoring (CGM) category.
Join as a T1D Warrior

Our T1D Warriors are children, parents of children with diabetes, and individuals living with type 1 diabetes who share their personal experiences to inspire and support others. Every story, every blog post, and every piece of advice you find here comes from someone who has truly lived it — with honesty, courage and a whole lot of heart. Together, we’re building a community where real-life experience truly makes a difference.
Want to inspire others with your T1D journey? Become a T1D Warrior and share your story.
