What Is Insulin?
Insulin helps your body turn food into energy and keeps your blood sugar in check. It’s a small hormone with a big job and knowing how it works can make a real difference for your health.
This content is not medical advice. Always consult your healthcare or diabetes care team before making any changes to your diabetes treatment or daily management.
How the Body Makes Insulin?
Insulin is a hormone made by special cells in the pancreas called beta cells. These cells are found in a part of the pancreas known as the islets of Langerhans.
The process of making insulin happens in a few steps, but what’s most important is that the body ends up producing insulin and another substance called C-peptide. These are released together.
Doctors often measure C-peptide in the blood because it stays in the body longer than insulin, which helps them see how much insulin the body is making naturally.
If you don’t have diabetes, your pancreas stores about 200 units of stored insulin. The body constantly releases small amounts of insulin, even when you’re not eating. After meals, this amount increases to help the body handle the sugar from food properly.
Why Insulin Is Essential?
Insulin is a vital hormone produced by beta cells in the pancreas. Its primary role is to regulate blood sugar (glucose) and keep the body’s energy system balanced. Insulin has three essential functions:
It helps glucose enter cells, where it’s used as energy.
It prevents the liver and muscles from producing and releasing too much sugar.
It inhibits the breakdown of fat into energy unless absolutely necessary.
What happens when there is no insulin?
Without insulin, glucose cannot enter the body’s cells especially muscle and fat cells so they signal that they’re “starving.” In response, the liver begins to release stored glucose (glycogen), thinking it’s helping. This makes blood sugar levels rise even more.
When blood glucose rises above 180 mg/dL ≈ 10 mmol/L, the kidneys try to flush out the excess sugar through urine. This leads to frequent urination and intense thirst, as large amounts of water are needed to eliminate glucose.
But that’s not all. Since cells can’t access glucose for energy, the body switches to burning fat and muscle instead. Breaking down fat produces ketones, which are acidic byproducts.
When cells can’t use glucose for energy, the body starts breaking down fat instead, producing acidic byproducts called ketones. If ketones build up in the blood, it can lead to diabetic ketoacidosis (DKA) a serious and potentially life-threatening condition.
Where Does the Insulin We Use Come From?
The insulin used by people with diabetes today is produced in several ways:
Human insulin – the most common type, made using recombinant DNA technology. A human insulin gene is inserted into bacteria or yeast, which then produce insulin. This type is very similar to natural human insulin and is widely used around the world.
Pork insulin – formerly extracted from pig pancreas. It is now used rarely, mostly by people who are sensitive to human insulin.
Beef insulin – once derived from cow pancreas, but it has been discontinued in most countries, including the U.S., due to a higher risk of allergic reactions and safety concerns.
Today, almost all newly diagnosed patients begin treatment with human insulin or insulin analogs, which are highly effective and safe.
Why Does Insulin Have to Be Injected?
Insulin is a protein. If taken by mouth, it would be broken down by the digestive system — just like the proteins we eat and wouldn’t reach the bloodstream in a usable form. That’s why insulin must be delivered through injections or pumps, directly into the body.
There is one exception: a form of inhalable insulin called Afrezza. It’s a fast-acting insulin that is inhaled before meals using a special device. However, it’s not suitable for everyone and doesn’t replace long-acting (basal) insulin. It is not recommended for people with asthma, lung disease, or for those who smoke.
In most cases, injectable insulin remains the safest and most effective way to manage type 1 diabetes.
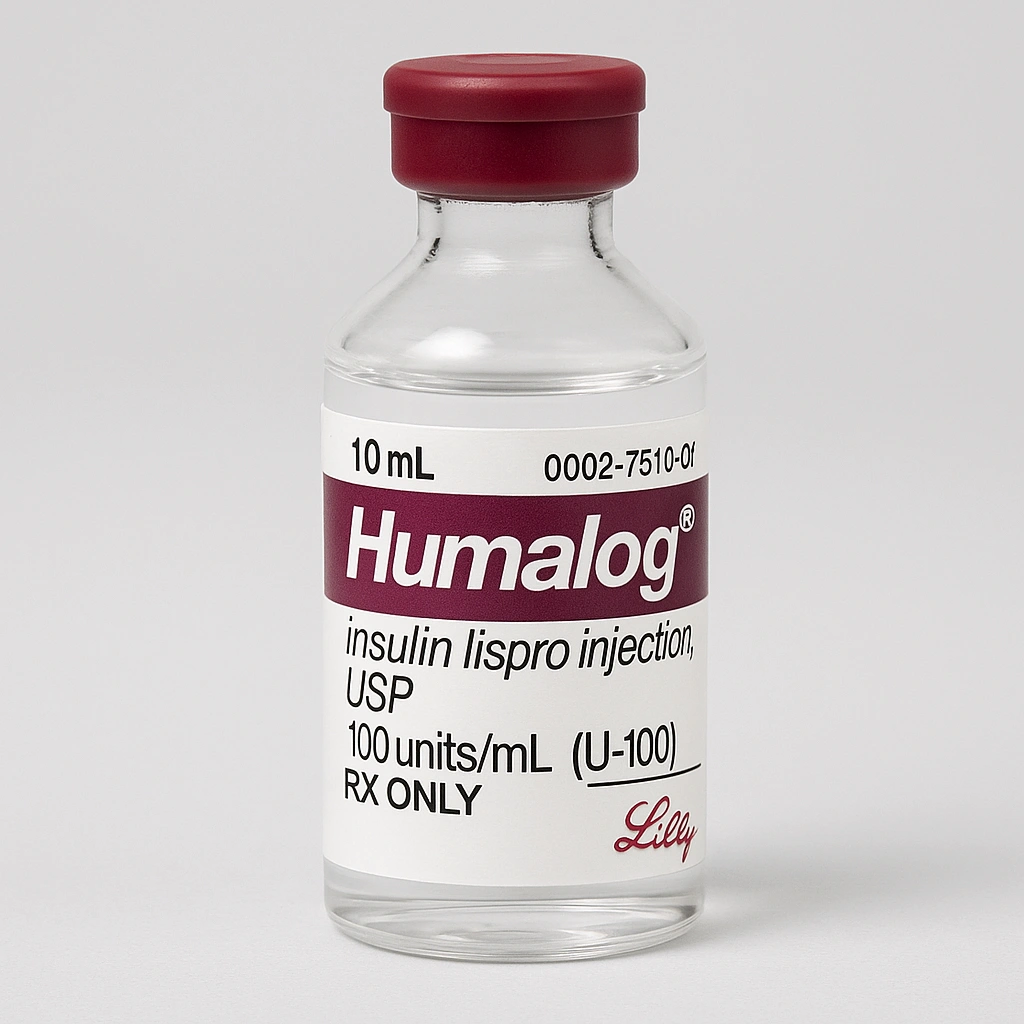
How to Store Insulin?
Unopened insulin vials or pens should be kept in a cool place, ideally in the refrigerator (between 2°C and 8°C). This helps preserve their effectiveness and extend shelf life.
Important: Never freeze insulin! Freezing can permanently damage it and make it ineffective.
Opened insulin (whether in a vial or pen) can be stored at room temperature, but only for 28 to 30 days, depending on the manufacturer. After that time, even if insulin remains, its effectiveness is no longer guaranteed and it should be discarded.

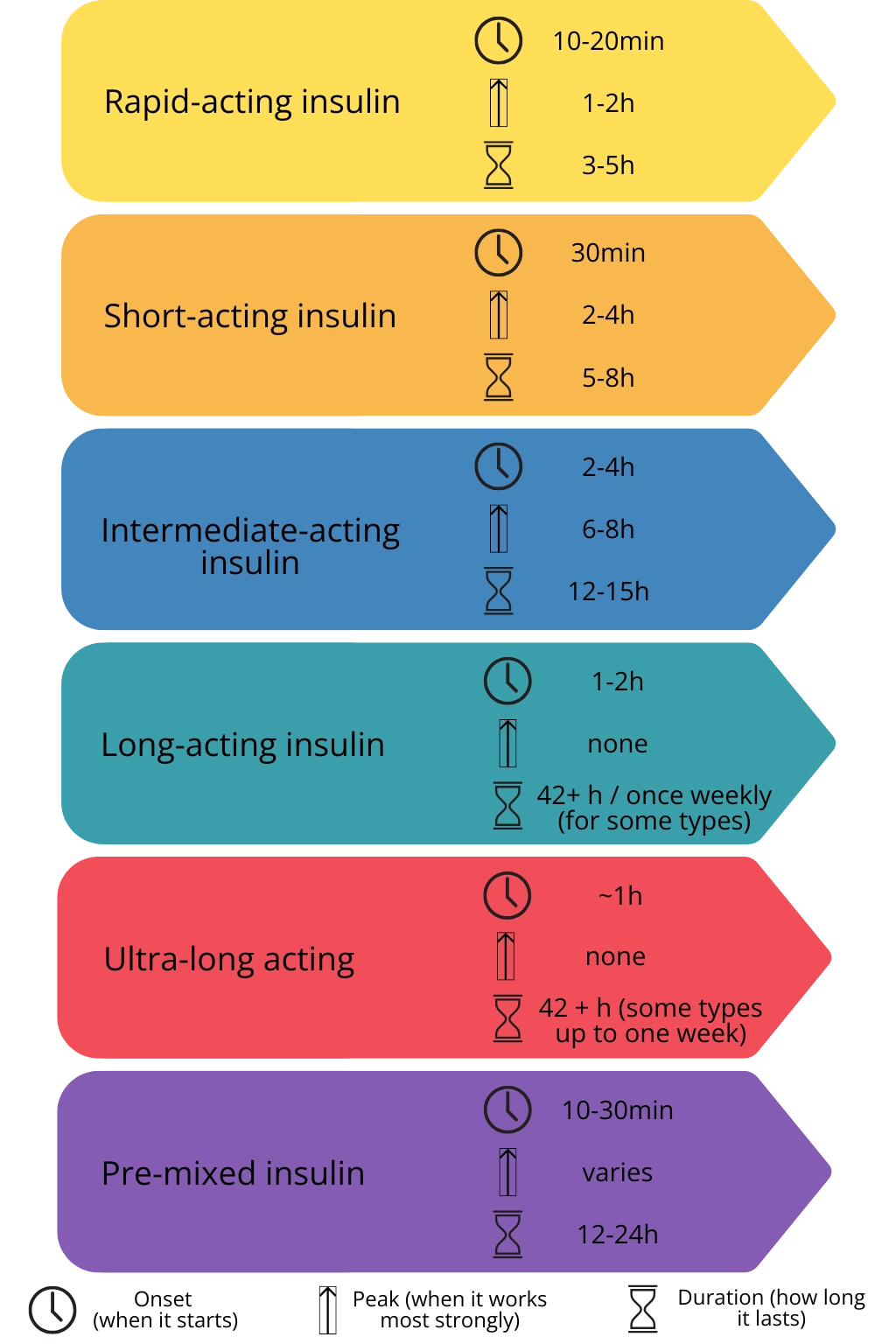
Types of Insulin and Their Differences
Insulins differ in how quickly they begin to work, when they reach their peak effect, and how long they last in the body. Here’s a basic overview:
Rapid-acting insulin
Starts working within minutes. Used around mealtimes to control blood sugar spikes after eating.Short-acting insulin
Takes a bit longer to start working than rapid-acting insulin. Also used before meals but less common today due to newer alternatives.Intermediate-acting insulin
Has a slower onset and longer duration. Often used to provide basal (background) insulin throughout the day or night.Long-acting insulin
Provides steady insulin levels with no pronounced peak. Typically taken once daily to maintain baseline glucose control.Ultra-long-acting insulin
Lasts more than 24 hours. Some types are designed for once-weekly injection to ensure consistent, long-term control.Pre-mixed insulin
Combines rapid- or short-acting with intermediate-acting insulin. Covers both mealtime needs and baseline requirements.
The types and availability of insulin can vary from country to country. For the most accurate and safe treatment plan, please consult your endocrinologist or healthcare provider. They can help you choose the most suitable insulin based on your individual needs, medical history and what is available in your region.
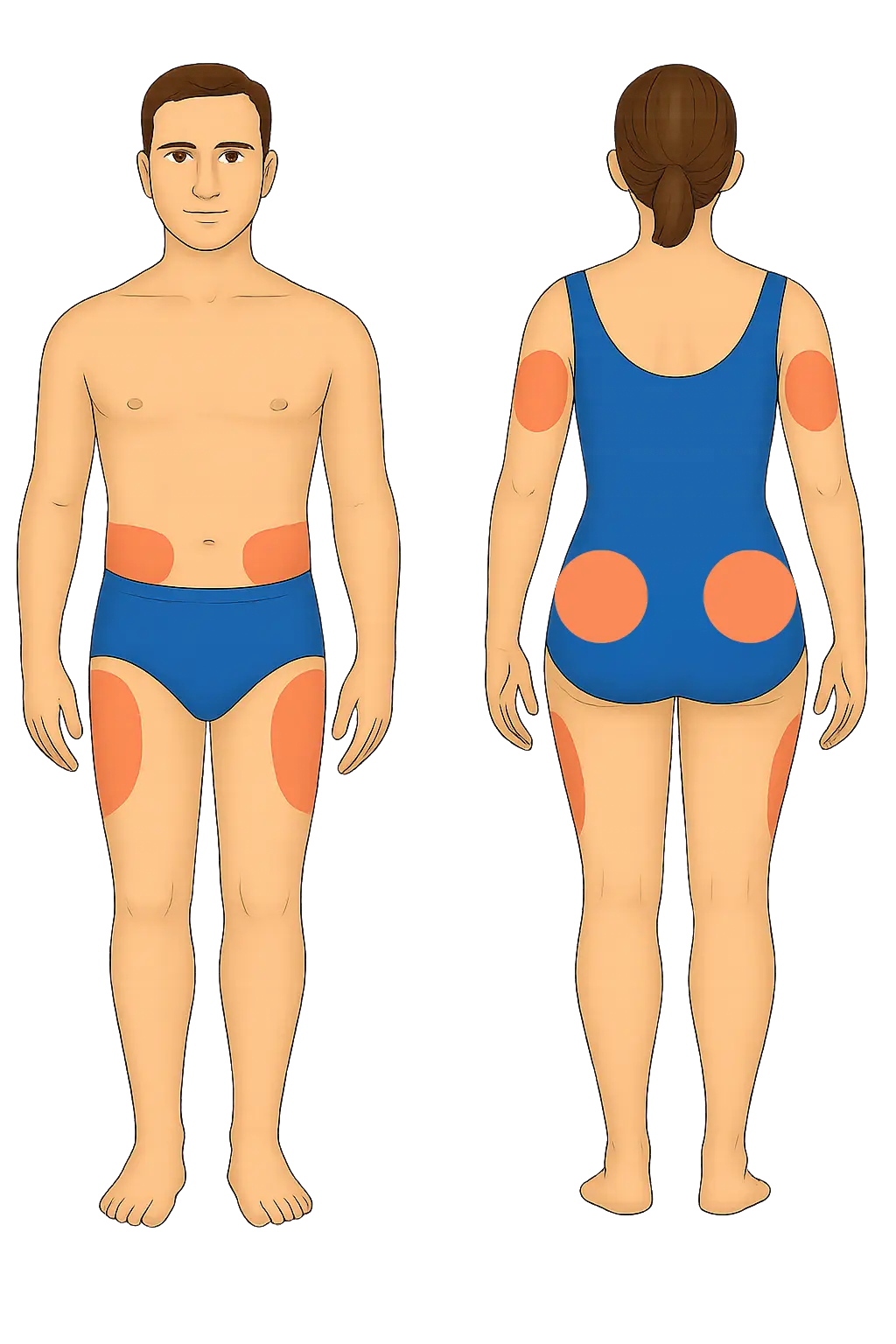
Where to Inject Insulin?
Subcutaneous (Sub-Q) Tissue
Insulin should always be injected into the subcutaneous tissue—the layer of fat just under the skin but above the muscle. This location ensures that insulin is absorbed at a steady and predictable rate, helping you maintain blood sugar control.
Although sub-Q tissue exists all over the body, certain areas are preferred for insulin injections because they are safer and offer better absorption, being far from large blood vessels or nerves.
Best Injection Sites:
Abdomen (at least 2 inches away from the belly button) – fastest absorption
Upper arms (back side, fatty area)
Front and sides of thighs
Buttocks
Site Rotation & Absorption
Injecting in the same spot over and over can lead to a condition called lipohypertrophy—a lump or buildup of fat under the skin. This can interfere with insulin absorption, making it less effective.
Why Rotate?
Prevents lipohypertrophy
Maintains consistent absorption
Reduces skin irritation
Rapid-acting insulin should be administered 10–15 minutes before a meal, as this timing ensures the best synchronization with glucose from the food.
If blood sugar is already elevated, the injection may need to be given slightly earlier.
Insulin administration should not be delayed too long after checking blood glucose or before a planned meal doing so may lead to hypoglycemia.
Always consider the current blood glucose level the dose and timing of insulin should be adjusted based on individual needs.
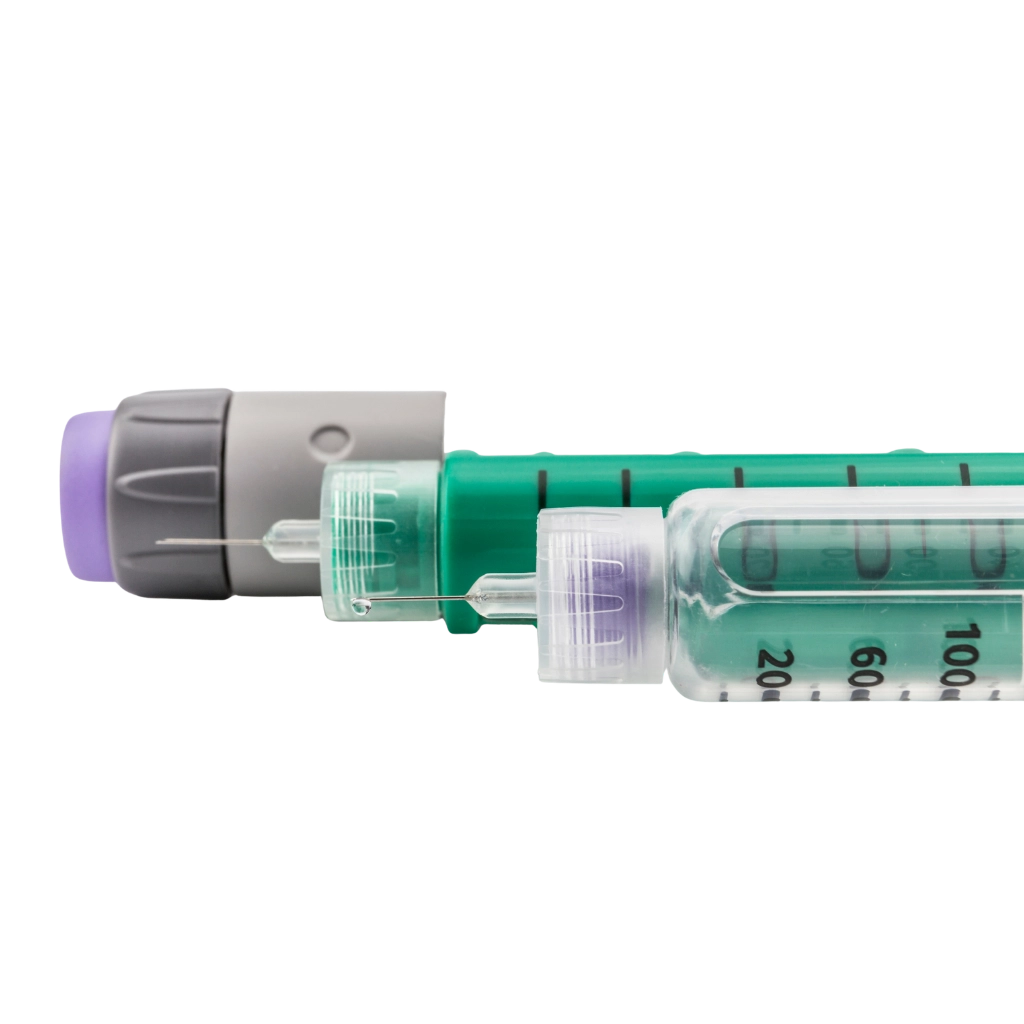
Insulin can be delivered in different ways. The most common are pens — both standard and smart pens that simplify daily use and insulin pumps, which provide continuous insulin delivery through a small device worn on the body.
You can learn more in our dedicated guides: Insulin Pens and Smart Pens and Insulin Pump Therapy.
Join as a T1D Warrior

Our T1D Warriors are children, parents of children with diabetes, and individuals living with type 1 diabetes who share their personal experiences to inspire and support others. Every story, every blog post, and every piece of advice you find here comes from someone who has truly lived it — with honesty, courage and a whole lot of heart. Together, we’re building a community where real-life experience truly makes a difference.
Want to inspire others with your T1D journey? Become a T1D Warrior and share your story.
