Pre-Bolus
Taking insulin before a meal helps keep blood sugar levels more stable and prevents sharp spikes after eating. The right pre-bolus timing can significantly improve glucose control.
This content is not medical advice. Always consult your endocrinologist, doctor or diabetes care team before making any changes to your diabetes treatment or daily management.
What is a Pre-Bolus?
Pre-bolus refers to the practice of taking rapid-acting insulin some time before eating, rather than at the start of a meal or afterward. The goal is to allow the insulin to start working by the time carbohydrates begin raising blood glucose levels, resulting in better post-meal (postprandial) blood sugar control.
Studies and visual data from the UC San Diego Diabetes Institute show that aligning insulin action with the post-meal rise in blood glucose can significantly reduce glucose spikes especially when insulin is given 15–20 minutes before eating, a practice known as pre-bolusing.
Rapid-acting insulin typically begins working within 5–20 minutes, peaks in 30–90 minutes, and remains active for about 3.5 to 5 hours. This makes timing a critical factor for optimal glucose control.
The diagram to the right illustrates this effect, showing how insulin administered before a meal can more effectively counter the post-meal glucose rise.

How Long Before a Meal Should You Pre-Bolus?
There’s no one-size-fits-all rule. The right timing depends on:
- Your current blood glucose level
- The type of rapid-acting insulin you use
- The kind of meal you’re having (fast vs. slow carbs)
- Whether you’re using a pump or injections
General guidance:
If glucose is within target: pre-bolus 10–20 minutes before eating
If glucose is elevated: you may need 25–40 minutes
If glucose is low: wait until levels stabilize before bolusing
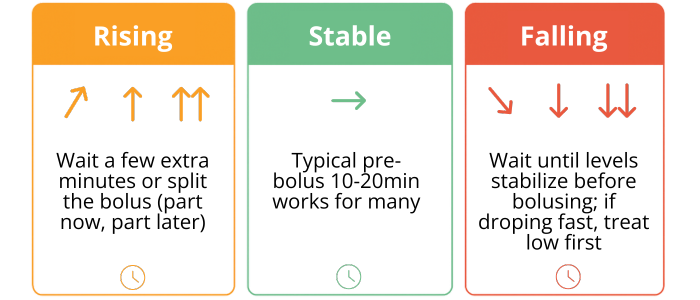
Optimizing Pre-Bolus Timing with CGM Trends
Finding the right pre-bolus timing can help keep post-meal glucose spikes under control. Use both your CGM trend arrows and a fingerstick check to guide your decision:
↗︎ or ↑ or (rising): If your CGM shows a rising glucose trend before a meal, giving the full bolus at once may cause your blood sugar to drop before the food begins to take effect. In these situations, it can sometimes help to split the dose — give part of the insulin right away, and the rest once the trend stabilizes. This approach can help avoid rapid glucose swings and better match insulin action to the post-meal rise.
→ (stable): If your glucose is steady, a standard pre-bolus of about 10–20 minutes before eating is often a good choice. This allows insulin to start working in time to blunt the post-meal spike.
↘︎ or ↓ (falling): If your glucose is dropping, giving insulin immediately may lower your blood sugar even further. In this case, wait until your levels stabilize, and if needed, have a small snack or fast-acting carbs first.
Fingerstick checks are especially useful if your CGM reading seems off or if the trend arrow changes quickly. Keep in mind that different CGM devices display trend arrows differently, so make sure you know what they mean on your specific device.
Timing will vary for each individual. Always discuss your pre-bolus timing adjustments with your endocrinologist or diabetes care team to ensure safety and effectiveness.

How to Find Your Ideal Pre-Bolus Timing?
It takes trial and error. Here’s how to start:
1. Track your pre and postmeal glucose levels.
2. Document your timing, insulin dose, food type and results.
3. Use CGM data (if available) to identify patterns.
4. Adjust timing slowly — don’t rush the process.
5. Talk to your healthcare team before making major changes.
With consistency, pre-bolusing becomes an effective tool in your daily diabetes routine.
Insulin action and timing can vary from person to person. Always consult your healthcare provider to determine what works best for you.
When Not to Pre-Bolus
There are times when pre-bolusing may not be appropriate, such as:
- When your blood sugar is low or trending downward
- When you’re not sure when food will be served (e.g., at restaurants)
- When you’re eating high-fat or slow-digesting meals
- If you live with gastroparesis or hypoglycemia unawareness
In these cases, consider alternative strategies like split boluses or extended boluses (if using an insulin pump).
Optimizing Pre-Bolus Correction as Part of Pre-Bolus Planning
If your glucose is above target before a meal, you may need to add a correction dose to your pre-bolus. This is extra insulin given to bring glucose back into range on top of covering your planned carbs.
The correction amount is usually based on your insulin sensitivity factor (ISF) and how much above target you are. If you’ve taken insulin recently, consider the insulin on board to avoid stacking.
The safest approach is to determine this together with your endocrinologist or diabetes care team.
Join as a T1D Warrior

Our T1D Warriors are children, parents of children with diabetes, and individuals living with type 1 diabetes who share their personal experiences to inspire and support others. Every story, every blog post, and every piece of advice you find here comes from someone who has truly lived it — with honesty, courage and a whole lot of heart. Together, we’re building a community where real-life experience truly makes a difference.
Want to inspire others with your T1D journey? Become a T1D Warrior and share your story.
