Understanding Type 1 Diabetes
Successful diabetes management isn’t just about insulin or treatment — it’s also about knowledge.
Understanding the basic concepts and processes can help you make more confident and calmer decisions in everyday life.
This content is not medical advice. Always consult your endocrinologist, doctor or diabetes care team before making any changes to your diabetes treatment or daily management.
What is Type 1 Diabetes?
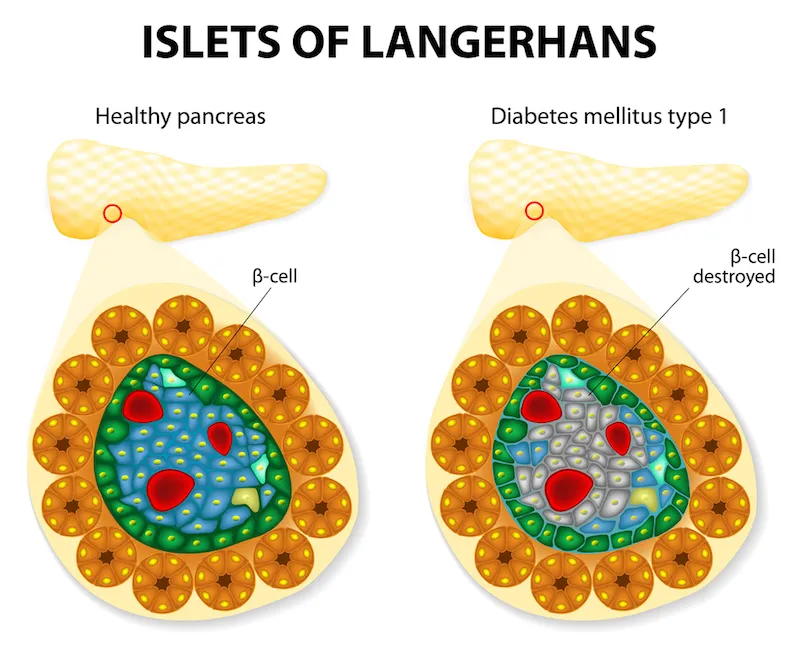
Type 1 diabetes is an autoimmune disease in which the immune system mistakenly destroys the pancreas cells that produce insulin. Without insulin, the body cannot use glucose from the blood for energy, and high blood sugar levels can become life-threatening. People with type 1 diabetes must take insulin every day through injections or an insulin pump, because their body cannot produce it on its own.
According to the World Health Organization, around 9 million people worldwide live with type 1 diabetes (2017 data). The most recent estimates from 2021 indicate that approximately 8.4 million people are affected, with about 500,000 new cases reported that year. Of those affected, 18% are children and adolescents.
In Europe, according to IDF data, about 295,000 children and young people live with type 1 diabetes, and more than 31,000 new cases are diagnosed each year in this age group. Europe has the highest number of young people with this condition compared to other regions.
It’s important to emphasize that type 1 diabetes is not caused by diet, obesity, or lifestyle. Its cause lies in a combination of genetic and environmental factors. It cannot be prevented or cured, but it can be successfully managed with insulin and proper care.
Type 1 diabetes is not the same as type 2 diabetes. While type 1 is an autoimmune condition and most commonly diagnosed in children and young adults, type 2 is more common in adults and is often linked to insulin resistance, excess weight, and lifestyle factors. Type 2 diabetes can sometimes be managed with healthy eating, physical activity, and oral medications, while people with type 1 diabetes will always require insulin.


Differences Between Type 1 and Type 2 Diabetes
Although both types of diabetes cause high blood sugar and require careful monitoring, they differ in their causes, how they develop, treatment approaches, and possibilities for prevention. Understanding these differences helps improve disease management and avoid misconceptions.
1. Cause
Type 1 Diabetes: An autoimmune disease in which the immune system mistakenly attacks and destroys the beta cells of the pancreas that produce insulin. Without insulin, the body cannot use glucose from the blood for energy.
Type 2 Diabetes: The body becomes resistant to insulin or does not produce enough of it. It is often linked to excess body weight, physical inactivity, and aging, but genetics also plays a significant role.
2. Age of Onset
Type 1: Most often develops in childhood or adolescence but can occur at any age. Onset is usually sudden, with pronounced symptoms.
Type 2: Most common in adults over the age of 40, but increasingly seen in younger people and even children due to rising obesity rates and unhealthy habits. Symptoms develop gradually and often go unnoticed at first.
3. Insulin Production
Type 1: The pancreas completely stops producing insulin. Insulin therapy is essential for survival.
Type 2: The pancreas still produces insulin, but the body does not use it effectively (insulin resistance). In later stages, insulin production may drop significantly.
4. Treatment
Type 1:
Insulin (injections or pump) – required for life.
Regular blood sugar monitoring (glucose meter or CGM).
- Education and planning for nutrition, physical activity, and stress management.
Type 2:
- Lifestyle changes (diet, physical activity).
- Oral medications or injections to improve insulin sensitivity.
- In some cases – insulin.
5. Prevention
Type 1: Cannot be prevented, as it is caused by an autoimmune process.
Type 2: Can often be prevented or delayed with proper diet, regular exercise, and maintaining a healthy body weight.
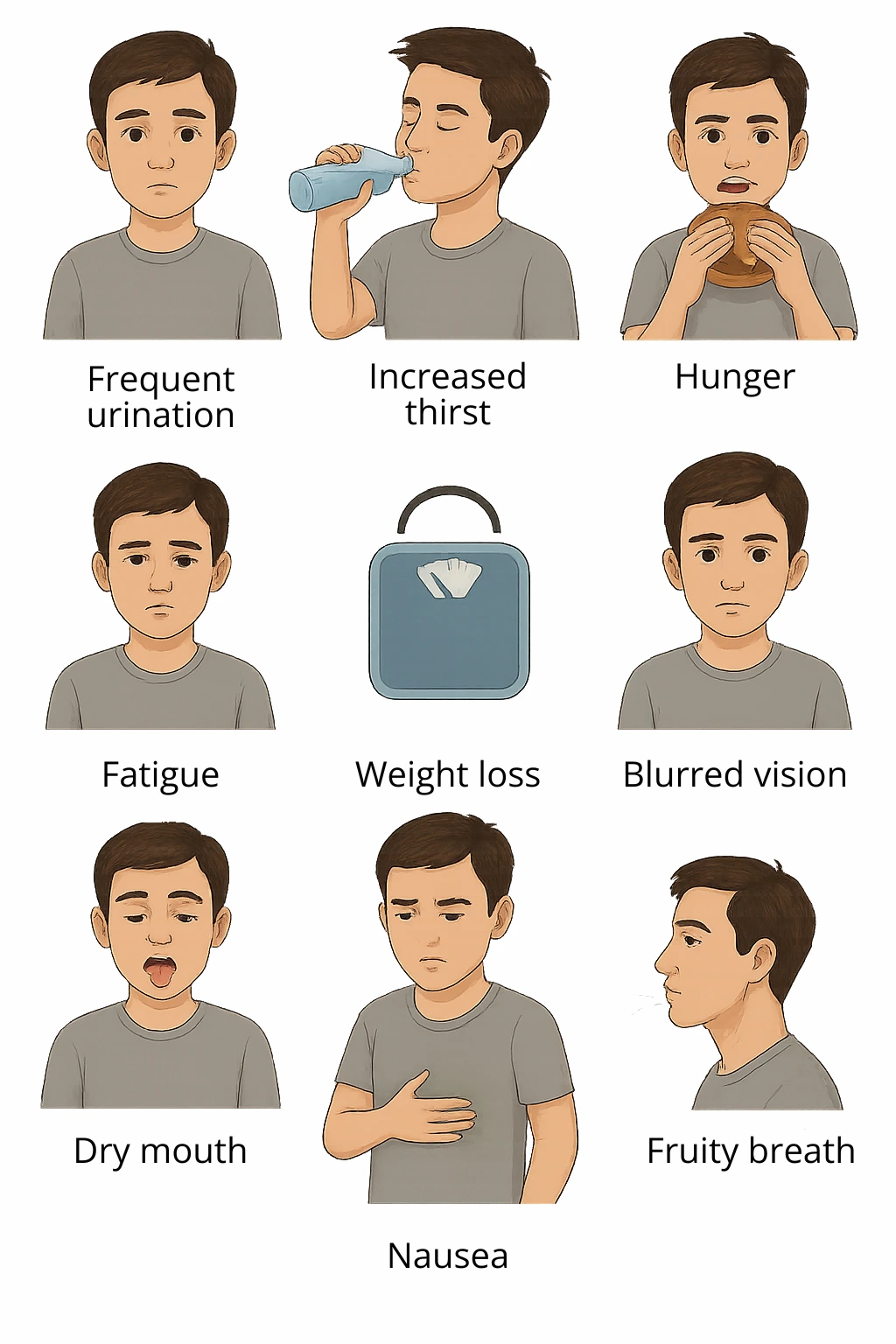
Symptoms of Type 1 Diabetes
Type 1 diabetes often appears suddenly, and symptoms become noticeable when most of the insulin-producing cells (beta cells) in the pancreas are already destroyed. Once the body can no longer regulate blood sugar levels, a set of recognizable signs begins to appear and it’s important to catch them early.
The most common symptoms include:
Increased thirst, even when drinking plenty of fluids
Frequent urination, especially at night
Increased appetite, often combined with unexplained weight loss
Fatigue and weakness without a clear cause
Blurred vision
Dry mouth and signs of dehydration
Sweet or fruity-smelling breath (especially in cases of ketoacidosis)
Nausea and vomiting
Confusion, drowsiness, and in more serious cases, fainting
Rapid and deep breathing (also known as Kussmaul breathing)
Fungal infections in girls, including infants and toddlers
Bedwetting, especially in children who were previously dry at night
Presence of sugar and ketones in the urine (usually confirmed by testing)
Symptoms can develop quickly — within days or weeks. That’s why it’s essential to act promptly if several of these signs appear at the same time, especially in children and young people.
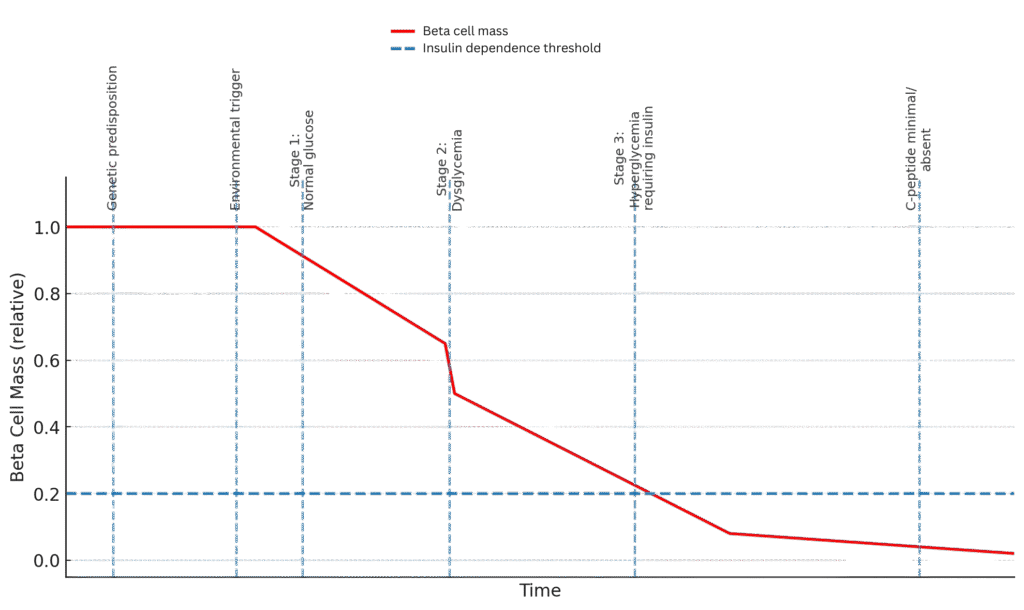
Although the symptoms appear suddenly, the actual development of the disease takes much longer.
In the background, the immune system slowly destroys the insulin-producing cells in the pancreas over months or even years, until the body can no longer regulate blood sugar and that’s when the symptoms suddenly appear.
If you suspect that you, your child, or another close person has diabetes, contact your doctor immediately.
Untreated type 1 diabetes can lead to a serious condition called diabetic ketoacidosis, which can be life-threatening.
What Causes Type 1 Diabetes?
Type 1 diabetes doesn’t develop overnight. While symptoms often appear suddenly, the disease itself progresses gradually over many years. Research including studies from the Joslin Diabetes Center has shown that changes in the body can begin up to nine years before the first symptoms appear.
The development of type 1 diabetes can be understood in several stages:
Genetic predisposition
A person may inherit genes that increase the risk of autoimmune activity. However, this doesn’t mean they will definitely develop the disease. Many people with these genes never develop diabetes.Environmental trigger
An infection, stress, or another environmental factor may trigger the immune system to begin reacting against the body’s own cells.Onset of autoimmunity
The immune system starts attacking the beta cells in the pancreas that produce insulin. This phase is silent — there are no visible symptoms — but diabetes-related antibodies can be detected in the blood.Gradual beta-cell destruction
Over time, the number of insulin-producing cells declines. The body struggles more and more to regulate blood sugar. There may still be no clear symptoms, but blood glucose levels may start to rise.Onset of type 1 diabetes symptoms
When more than 90% of beta cells are destroyed, the body can no longer regulate blood sugar on its own. This is when classic symptoms appear: excessive thirst, frequent urination, fatigue, weight loss, and others.
Type 1 Diabetes and Life Inside the Pancreas
Although type 1 diabetes is often viewed as a complete shutdown of insulin production, new insights tell a more nuanced story. In some individuals who have lived with the disease for many years, small but measurable amounts of C-peptide — a byproduct released along with insulin can still be detected. This suggests that some beta cells may still be functioning, at least partially.
This raises an important question: is the body still trying to generate new islet cells, even under continuous autoimmune attack?
While the answers are not yet definitive, studies suggest that preserved or regenerated pancreatic activity may help reduce the risk of complications, improve blood sugar stability, and contribute to a better quality of life. These findings are reshaping our understanding of type 1 diabetes and encouraging new research into therapies that not only replace insulin but also aim to protect what the body still has.
Understanding disease progression also helps explain why some people may still have small amounts of insulin production years after diagnosis. Even after the immune system has destroyed most of the beta cells, some may survive or partially recover. These remaining cells can continue to produce small amounts of insulin, which is often detected through C-peptide testing. In some cases, the pancreas may even attempt to regenerate new beta cells, although the ongoing autoimmune attack usually limits this process. This residual insulin production can help smooth out blood sugar fluctuations, reduce insulin requirements, and may be linked to a lower risk of diabetes complications.
Most people with type 1 diabetes carry certain genes that increase their risk, but genetics alone don’t cause the disease. Environmental factors such as viral infections are often needed to trigger the autoimmune process.
Risk Factors for Type 1 Diabetes
People with type 1 diabetes typically have a genetic predisposition, but the disease usually develops only when multiple factors come together. Studies on identical twins show that if one twin has T1D, the other develops it only in 30–50% of cases — clearly indicating that genetics alone is not enough (Cell Genomics, 2025).
If one parent has type 1 diabetes, the child’s risk is approximately:
6–7% if the father is affected,
1.5–2.5% if the mother is affected.
If both parents have type 1 diabetes, the risk is significantly higher.
Risk can be further refined through HLA typing on chromosome 6. Some gene patterns increase risk, while others are considered protective.
As for environmental factors, studies like TEDDY and DIPP suggest that viral infections, especially Coxsackie B virus, may act as triggers that initiate the autoimmune process in genetically susceptible individuals.
Once triggered, the immune system produces autoantibodies, which can be detected months or even years before symptoms appear.
Summary of Key Findings:
Genetic predisposition alone is not enough.
Risk is higher in families with a history of type 1 diabetes, especially from the father.
Identical twins don’t always both develop T1D — highlighting the role of the environment.
Autoantibodies can be detected well before symptoms appear.
Viral infections, especially Coxsackie B, are considered potential triggers.
HLA typing helps estimate individual genetic risk.

How Is Type 1 Diabetes Treated?
The main goal of type 1 diabetes treatment is to keep blood sugar levels within a healthy range and prevent both short-term and long-term complications. Because the pancreas can no longer produce insulin, this hormone must be supplied from outside the body. Insulin therapy is therefore the foundation of treatment — without it, survival is not possible.
Treatment usually combines:
Insulin therapy – delivered through multiple daily injections or an insulin pump to mimic natural insulin release.
Blood glucose monitoring – using fingerstick tests or continuous glucose monitoring (CGM) systems to track levels in real time.
Healthy lifestyle choices – balanced nutrition, regular physical activity, and attention to overall wellbeing.
Education and self-management skills – learning how to adjust insulin doses, count carbohydrates, and respond to high or low blood sugar readings.
Advances in diabetes technology such as CGMs, smart insulin pens, and hybrid closed-loop pump systems — are making it easier to keep blood sugar in target ranges and reduce the burden of daily management.
For more about how insulin works and why it’s essential in type 1 diabetes care, you can learn more here.
Why Does Insulin Have to Be Injected?
Insulin is a protein. If taken by mouth, it would be broken down by the digestive system — just like the proteins we eat and wouldn’t reach the bloodstream in a usable form. That’s why insulin must be delivered through injections or pumps, directly into the body.
There is one exception: a form of inhalable insulin called Afrezza. It’s a fast-acting insulin that is inhaled before meals using a special device. However, it’s not suitable for everyone and doesn’t replace long-acting (basal) insulin. It is not recommended for people with asthma, lung disease, or for those who smoke.
In most cases, injectable insulin remains the safest and most effective way to manage type 1 diabetes.
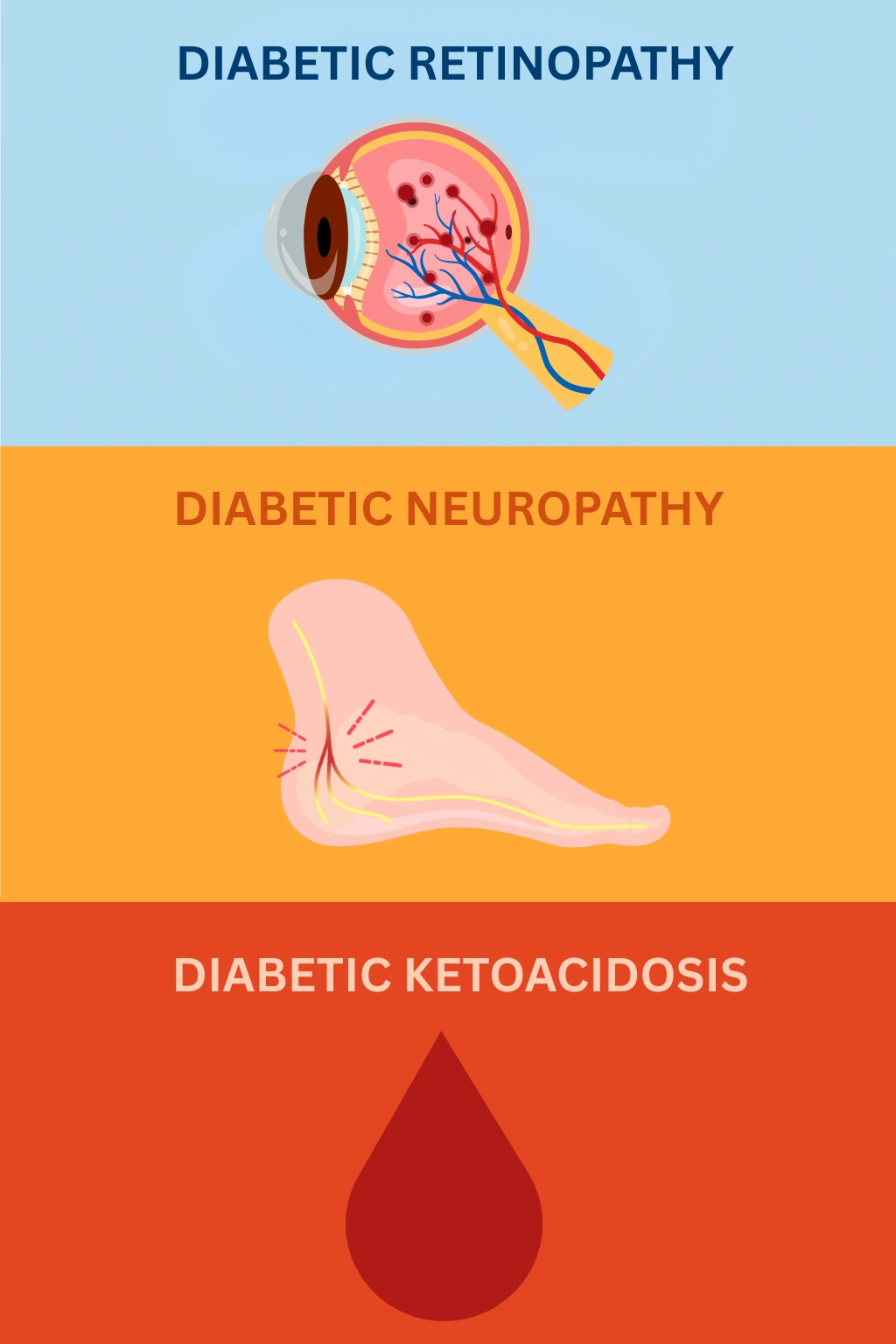
Complications and the Importance of Good Control
Type 1 diabetes is a lifelong condition that can affect nearly every organ system in the body. Over time, persistently high blood sugar (hyperglycemia) damages blood vessels and nerves, which increases the risk of both short-term emergencies and long-term complications.
Diabetic retinopathy – Long-term high blood sugar can weaken and damage the tiny blood vessels in the retina, the light-sensitive tissue at the back of the eye. This may lead to blurred vision, dark spots, or even complete loss of vision. Regular eye exams and good glucose control are essential to prevent or slow down this complication.
Diabetic neuropathy – Excess sugar in the blood can injure nerve fibers, particularly in the extremities. This often begins in the feet and legs but can also affect the hands. Symptoms include tingling, burning, pain, or numbness, which may lead to unnoticed injuries or infections.
Diabetic ketoacidosis (DKA) – This is an acute, life-threatening complication that occurs when the body cannot access glucose for energy due to a lack of insulin. Instead, it breaks down fat, producing ketones, which make the blood acidic. DKA can develop within hours, especially during illness or missed insulin doses, and requires urgent medical care.
Other possible complications:
Diabetic nephropathy – kidney damage that can lead to chronic kidney disease or kidney failure.
Cardiovascular disease – higher risk of heart attack, stroke, and poor circulation.
Foot problems – ulcers, infections, or even amputations due to nerve damage and poor blood flow.
Skin conditions – bacterial or fungal infections, slow-healing wounds.
Oral health issues – gum disease and other dental problems.
Maintaining stable blood sugar levels with insulin therapy, healthy lifestyle choices, and regular medical check-ups greatly reduces the risk of all these complications, helping protect long-term health and quality of life.
Join as a T1D Warrior

Our T1D Warriors are children, parents of children with diabetes, and individuals living with type 1 diabetes who share their personal experiences to inspire and support others. Every story, every blog post, and every piece of advice you find here comes from someone who has truly lived it — with honesty, courage and a whole lot of heart. Together, we’re building a community where real-life experience truly makes a difference.
Want to inspire others with your T1D journey? Become a T1D Warrior and share your story.
