High Blood Sugar (Hyperglycemia)
Consistently high blood sugar can cause serious damage which is why regular monitoring and good management are key to staying healthy.
This content is not medical advice. Always consult your endocrinologist, doctor or diabetes care team before making any changes to your diabetes treatment or daily management.
What Is High Blood Sugar (Hyperglycemia)?
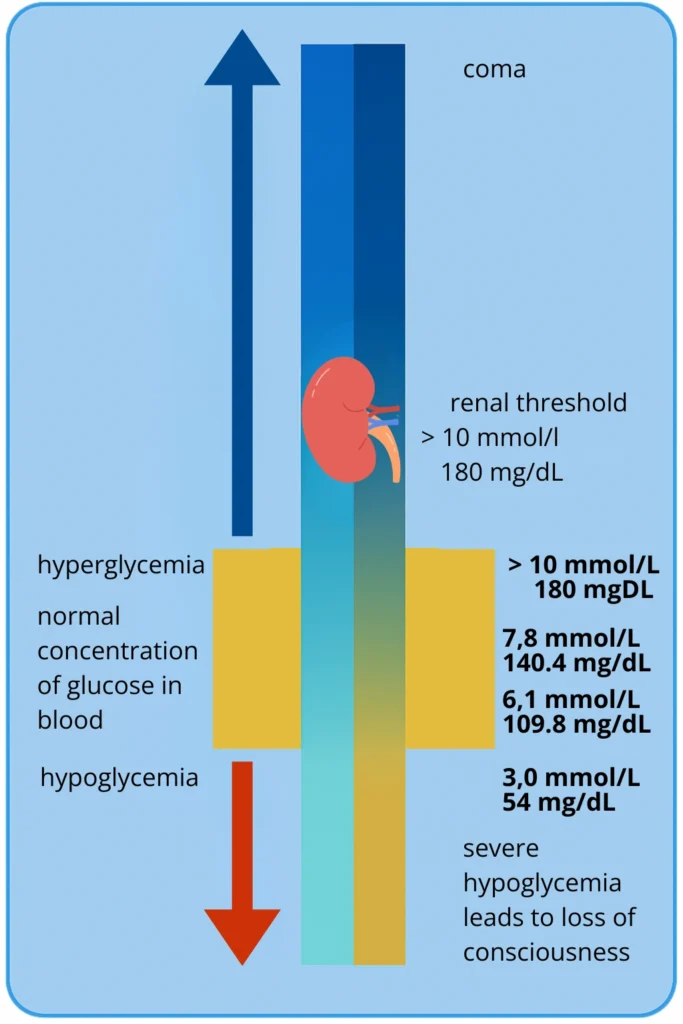
Hyperglycemia is the medical term for elevated blood glucose (sugar) levels. In people with type 1 diabetes, it means the body doesn’t have enough insulin, or the insulin isn’t working effectively, causing glucose to remain in the bloodstream instead of entering the cells to be used for energy.
Blood sugar can rise occasionally (for example, after a meal), but if it stays high for longer periods or happens frequently, it can cause serious damage to blood vessels, eyes, kidneys, and nerves.
Hyperglycemia isn’t always immediately dangerous, but it should never be ignored. Understanding its causes and responding in time can help prevent serious complications, such as diabetic ketoacidosis (DKA) which requires urgent medical treatment.
Causes of Hyperglycemia
In people with type 1 diabetes, hyperglycemia most often occurs when there’s not enough insulin in the body. This can happen for many reasons — sometimes it’s due to a missed dose, an unexpected meal, or technical issues like a blocked insulin pump or a dislodged infusion set.
High blood sugar is also common during periods of illness, fever, or emotional stress. In these situations, the body releases stress hormones that increase blood glucose levels, which may mean more insulin is needed than usual.
Other factors that can contribute to hyperglycemia include:
Eating carbohydrate-rich foods without taking enough insulin
Lack of physical activity
Improper insulin injection or using expired insulin
Medications like steroids (e.g., corticosteroids)
Hormonal changes (puberty, menstruation)
Emotional strain or anxiety
It’s important to understand that hyperglycemia doesn’t always mean someone has “done something wrong.” It’s a natural part of life with type 1 diabetes. What matters is recognizing it early and understanding why it happened, so that next time, you can respond quickly and confidently.
Hyperglycemia symptoms don’t appear the same way in everyone. Some people may notice them quickly, while for others they may remain unnoticed until the condition becomes more serious. Regular glucose monitoring, recognizing patterns and responding quickly to changes can help prevent complications.
Signs and Symptoms of Hyperglycemia
In the early stages, hyperglycemia can go unnoticed, especially if blood sugar isn’t measured regularly. However, as glucose levels rise and stay elevated, symptoms begin to appear and become more noticeable.
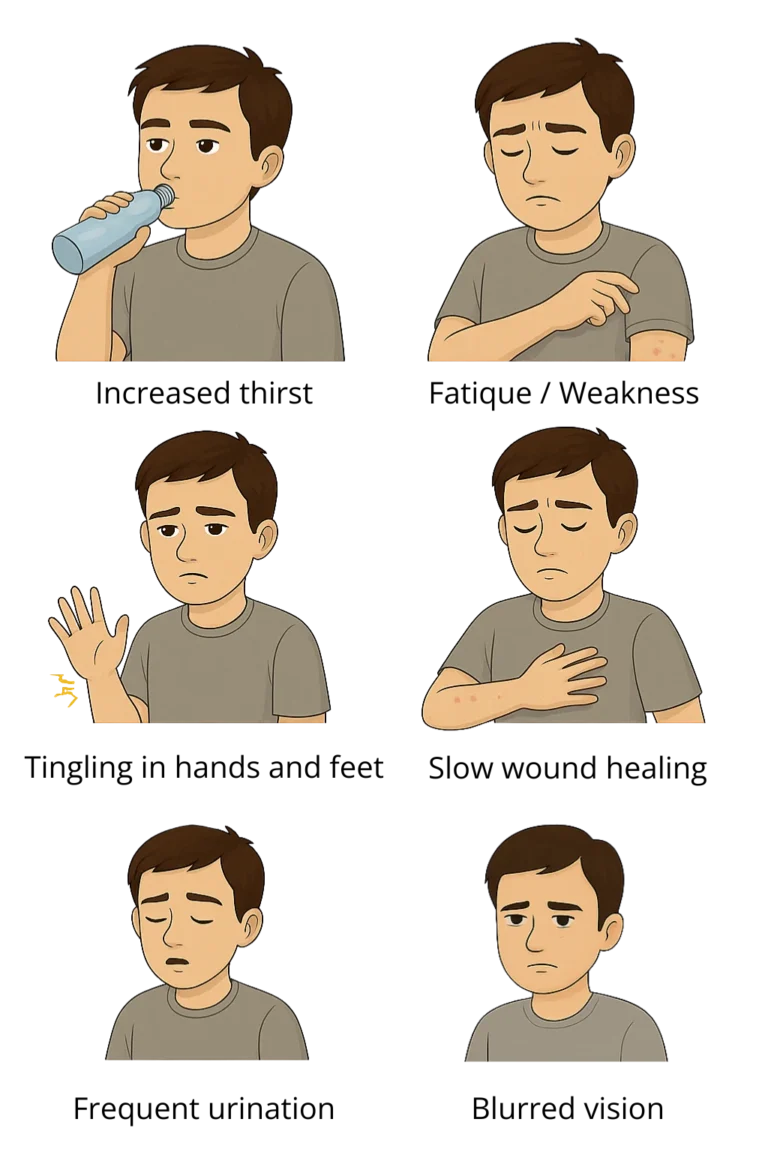
Early Signs of Hyperglycemia:
These symptoms develop gradually and are often overlooked because they don’t seem serious, but they’re the first indication that blood sugar is out of control:
Increased thirst (polydipsia): The body tries to compensate for fluid loss caused by frequent urination.
Frequent urination (polyuria): Excess glucose is filtered through the kidneys and excreted via urine, leading to dehydration.
Dry mouth and skin: Dehydration from fluid loss causes mucous membranes and skin to dry out.
Fatigue and weakness: Cells aren’t getting enough glucose for energy, leading to exhaustion.
Blurred vision: High blood sugar can affect the eye lens, temporarily impairing vision.
Progressive Symptoms (when hyperglycemia persists):
If high blood sugar isn’t recognized and treated promptly, symptoms worsen and become more persistent:
Tingling, burning, or numbness in hands and feet: Prolonged high glucose can damage nerves (diabetic neuropathy).
Slow healing of wounds and cuts: High sugar levels damage blood vessels, slowing circulation and tissue repair.
Increased appetite but weight loss: The body can’t use glucose properly, so it breaks down muscle and fat for energy.
Irritability and trouble concentrating: Blood sugar fluctuations affect the brain and mood.
How to Respond to and Treat Hyperglycemia?
High blood sugar isn’t always a reason to panic, but it does require timely and thoughtful action.
First steps when your blood sugar is too high:
Check your blood glucose level
If it’s above 10 mmol/L (180 mg/dL), increase the frequency of monitoring (every 2–3 hours).Test for ketones
If your glucose is above 13.3 mmol/L (240 mg/dL), check your urine or blood for ketones.Take a correction dose of rapid-acting insulin
This dose depends on your insulin sensitivity and the plan provided by your healthcare team. Typically, it’s about 10–20% of your total daily insulin dose.Drink water
Staying hydrated helps flush out excess glucose through urine.Avoid exercise if ketones are present
Physical activity in this state can worsen your condition and increase the risk of DKA.Recheck your blood sugar after 2 hours
If levels are still high or rising, contact your doctor.
Contact your healthcare provider if:
You feel that your current treatment may need adjustment.
You’ve measured high blood glucose levels 3 or 4 times in a row.
You’ve had 3 or more consecutive urine tests showing very high glucose levels.
You’ve recorded 2 or more high blood glucose readings within a 24-hour period.
You’ve noticed that your glucose levels are consistently high at the same time of day for several days.
All your glucose readings are higher than the target range agreed upon with your doctor.
Log your glucose readings, insulin doses and symptoms. This helps your doctor make better decisions about your care. Illness, stress or changes in routine can all cause your blood sugar to rise more easily. Be prepared and follow your treatment plan closely.
Diabetic Ketoacidosis (DKA)
Diabetic ketoacidosis (DKA) is a serious and potentially life-threatening complication of type 1 diabetes. It occurs when the body doesn’t have enough insulin and starts breaking down fat for energy. This process produces ketones acidic substances that can build up in the blood and cause the body to become dangerously acidic if not treated in time.
DKA most often develops when blood sugar is very high and ketones are present in the blood or urine. The condition can worsen quickly, especially during illness, infection, skipped insulin doses, or technical problems with an insulin pump.
Warning Signs of DKA:
Nausea and vomiting
Abdominal pain
Deep, rapid breathing (Kussmaul breathing)
Fruity-smelling breath (due to ketones)
Confusion or drowsiness
Loss of appetite
Extreme thirst and dehydration
Rapid heart rate
Loss of consciousness in severe cases
How to prevent DKA?
Never skip insulin, even if you’re not eating.
Check for ketones when your blood sugar is high or when you’re sick.
Follow your sick day management plan as advised by your doctor or diabetes educator.
If you experience nausea, vomiting, or can’t keep food or fluids down — don’t wait, go to the hospital.
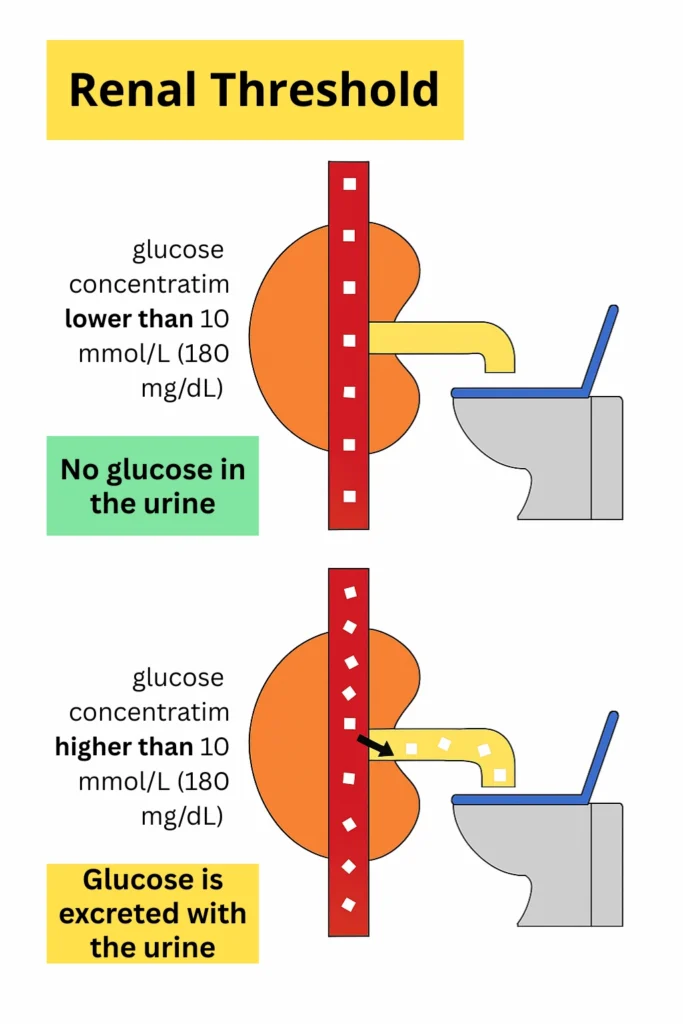
If your blood sugar is above 10 mmol/L (180 mg/dL), it’s important to monitor your glucose more frequently. Once it exceeds 13.3 mmol/L (240 mg/dL), you should check for ketones. The presence of ketones along with high blood sugar may indicate the early stages of diabetic ketoacidosis (DKA). Never exercise if ketones are present, as physical activity can make the condition worse. If you experience nausea, stomach pain, rapid breathing, or a fruity-smelling breath contact your doctor immediately.
Join as a T1D Warrior

Our T1D Warriors are children, parents of children with diabetes, and individuals living with type 1 diabetes who share their personal experiences to inspire and support others. Every story, every blog post, and every piece of advice you find here comes from someone who has truly lived it — with honesty, courage and a whole lot of heart. Together, we’re building a community where real-life experience truly makes a difference.
Want to inspire others with your T1D journey? Become a T1D Warrior and share your story.
