Blood Glucose Monitoring
Keeping track of blood sugar levels is a key part of living with type 1 diabetes. Whether you use a glucose meter or a CGM device, regular checks help you understand how your body responds to food, activity, and insulin so you can make safer, more confident choices every day.
This content is not medical advice. Always consult your endocrinologist, doctor or diabetes care team before making any changes to your diabetes treatment or daily management.
Blood Glucose Monitoring
Monitoring blood sugar levels is one of the most important aspects of managing type 1 diabetes and one of the most helpful. It helps you understand how your body reacts to food, exercise, insulin, stress, and illness. The more you learn from your numbers, the more confident you’ll feel in daily decisions.
Why it matters?
Your blood glucose (or blood sugar) levels show how much glucose is in your bloodstream at a given moment. Since people with T1D no longer produce insulin, they need to closely watch these levels and respond when they go too high or too low.
Consistent monitoring helps you:
Stay within your target range
Avoid hypoglycemia and hyperglycemia
Adjust your insulin doses more precisely
Understand patterns (like morning highs or activity-related lows)
Ways to Check Blood Sugar
Glucose Meter (Fingerstick)
A glucose meter measures your blood sugar using a small drop of blood from your fingertip. While it might sound intimidating at first, with time it becomes a simple part of your daily routine.
Step-by-Step Guide:
Make sure the area you’re testing is clean and completely dry. Any leftover moisture, such as water, juice, or lotion, can dilute the blood sample and lead to inaccurate results.
Use a fresh strip taken directly from its container or protective foil. Insert a test strip into your meter.
Gently massage the fingertip to stimulate blood flow and make it easier to collect a drop of blood. Use the lancing device and press it gently against the side of your fingertip.
Without pressing too hard, allow a small drop of blood to form on your fingertip.
Wait for the reading, usually takes around 5 seconds. After the reading is displayed, carefully remove the test strip from your device.
Many people use meters several times a day: before meals, after meals, before bed, and anytime they feel “off”.
When to test?
Many people with diabetes test multiple times a day, including:
Before meals
2 hours after meals
Before bedtime
When feeling symptoms of high or low blood sugar
Before and after exercise
Keeping track of these readings helps with day-to-day decisions about food, medication activity and gives your healthcare provider a better picture of your glucose trends over time.

Warm Water for Easier Blood Sampling
If your hands are cold, try warming them with warm water or rubbing them together before pricking. It will be easier to get a drop of blood, and the prick will hurt less.
Glucose monitoring routines may vary depending on the device you’re using including timing, method, and target ranges. These are only general guidelines. Always follow the instructions provided by your device manufacturer, and if you’re unsure about anything, speak with your diabetes care team, such as your endocrinologist or certified diabetes educator.

Continuous Glucose Monitor (CGM)
A CGM measures glucose levels automatically through a small sensor worn on the skin. Instead of fingersticks, it gives continuous readings every few minutes and alerts you to highs and lows.
Benefits of CGM:
Real-time updates
Fewer finger pricks
Customizable alarms
Trend arrows to show where your sugar is heading
CGMs are especially helpful for kids, active people, and those wanting more data to fine-tune their insulin use.
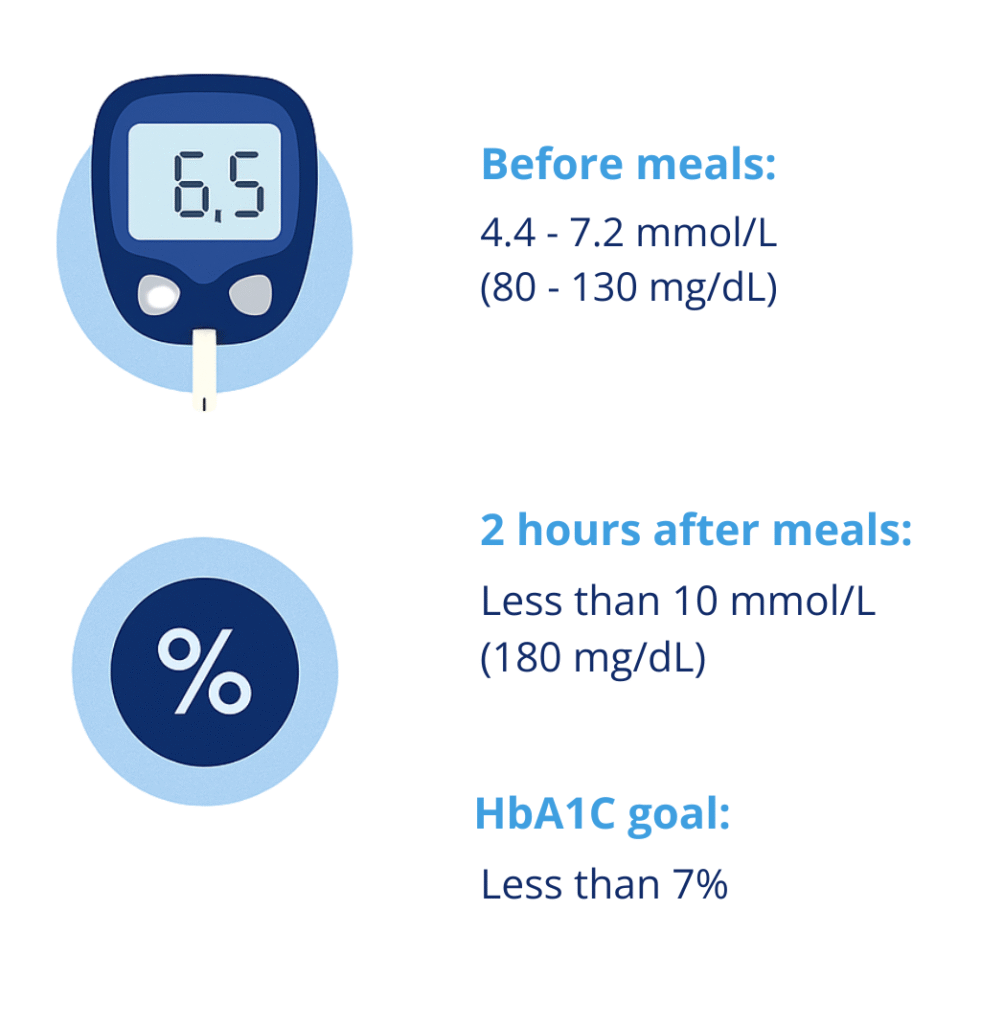
Target Ranges
Your ideal blood sugar range may vary depending on age, lifestyle, or doctor recommendations. These are general ADA guidelines:
Before meals: 4.4–7.2 mmol/L (80–130 mg/dL)
2 hours after meals: Less than 10 mmol/L (180 mg/dL)
HbA1C goal: Less than 7%
These are general targets recommended by diabetes associations, but your doctor may adjust them based on age, health status, or individual needs.
Remember every person with T1D is different. Your doctor or diabetes educator will help you define the right range for you or your child.
This raises an important question: is the body still trying to generate new islet cells, even under continuous autoimmune attack?
While the answers are not yet definitive, studies suggest that preserved or regenerated pancreatic activity may help reduce the risk of complications, improve blood sugar stability, and contribute to a better quality of life. These findings are reshaping our understanding of type 1 diabetes and encouraging new research into therapies that not only replace insulin but also aim to protect what the body still has.
The HbA1C test doesn’t measure your current blood sugar level — it shows the average over the past 3 months. It’s used as a long-term indicator of diabetes management.
Which Glucose Meters Are Available in Your Country?
There are many different glucose meters available on the market to help you monitor your blood sugar levels. However, the availability of specific devices can vary depending on the country and healthcare system. Before making a purchase, it’s important to check whether the glucose meter is:
Approved and authorized for use in your country (e.g., CE marked for the EU, FDA approved for the U.S., UKCA for the United Kingdom, TGA approved for Australia, etc.)
Covered by your health insurance or reimbursed through the public healthcare system
Suitable for your needs — whether you prefer a standard glucose meter, CGM (Continuous Glucose Monitor), or a more advanced system
Always consult your doctor, pharmacist, or diabetes educator before choosing a device, and make sure it’s compatible with your country’s regulations and your insurance plan.
Join as a T1D Warrior

Our T1D Warriors are children, parents of children with diabetes, and individuals living with type 1 diabetes who share their personal experiences to inspire and support others. Every story, every blog post, and every piece of advice you find here comes from someone who has truly lived it — with honesty, courage and a whole lot of heart. Together, we’re building a community where real-life experience truly makes a difference.
Want to inspire others with your T1D journey? Become a T1D Warrior and share your story.
